Dementia. It’s the word nobody wants to hear. It steals memories, erases personalities, and slowly disconnects people from the world they’ve spent a lifetime building. Today, over 55 million people worldwide live with dementia, and that number is expected to triple by 2050. But here’s what most people don’t understand: dementia isn’t a single disease. It’s an umbrella term for a group of brain conditions that destroy cognitive function — and each one attacks the brain in a different, terrifying way.
So why does dementia happen? Is it just “getting old”? Is it genetic destiny? Can you actually prevent it? The answers are more complex, more surprising, and more hopeful than you might think. Let’s break down what’s really happening inside the brain when dementia strikes — and what science says you can do about it.
1. The Toxic Protein Problem: Amyloid Plaques and Tau Tangles
The most common form of dementia is Alzheimer’s disease, accounting for 60-80% of all cases. And the primary villains in Alzheimer’s are two rogue proteins: beta-amyloid and tau. Understanding how these proteins go wrong is key to understanding why Alzheimer’s happens.
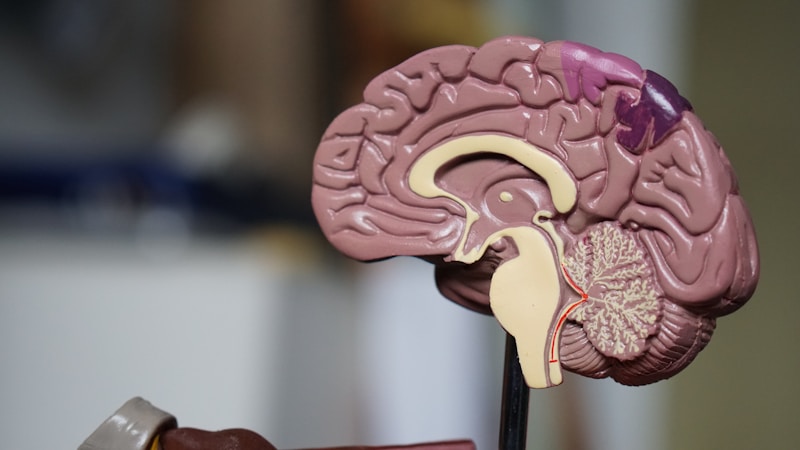
In a healthy brain, beta-amyloid is produced and cleared away regularly — it’s a normal byproduct of cell activity. But in Alzheimer’s, this cleanup process breaks down. Beta-amyloid proteins start clumping together into sticky amyloid plaques that accumulate between brain cells. These plaques act like biological roadblocks, disrupting communication between neurons and triggering an inflammatory immune response that damages surrounding tissue.
Meanwhile, inside the neurons themselves, another protein called tau starts malfunctioning. Normally, tau acts like railroad tracks inside cells, helping transport nutrients and essential materials. But in Alzheimer’s, tau proteins detach from their structure, twist into tangled threads called neurofibrillary tangles, and collapse the cell’s internal transport system. Without this transport network, neurons can’t communicate, can’t function, and eventually die. As billions of neurons die, the brain literally shrinks — sometimes losing up to 30% of its volume in advanced cases.
What triggers this cascade? Scientists believe it starts decades before symptoms appear. The amyloid buildup may begin 15-20 years before a person notices any memory problems. By the time someone is diagnosed, massive damage has already occurred. This is why early detection and prevention research is so critical — by the time you notice symptoms, the brain has been under attack for years.
2. Vascular Dementia: When Blood Flow to the Brain Breaks Down
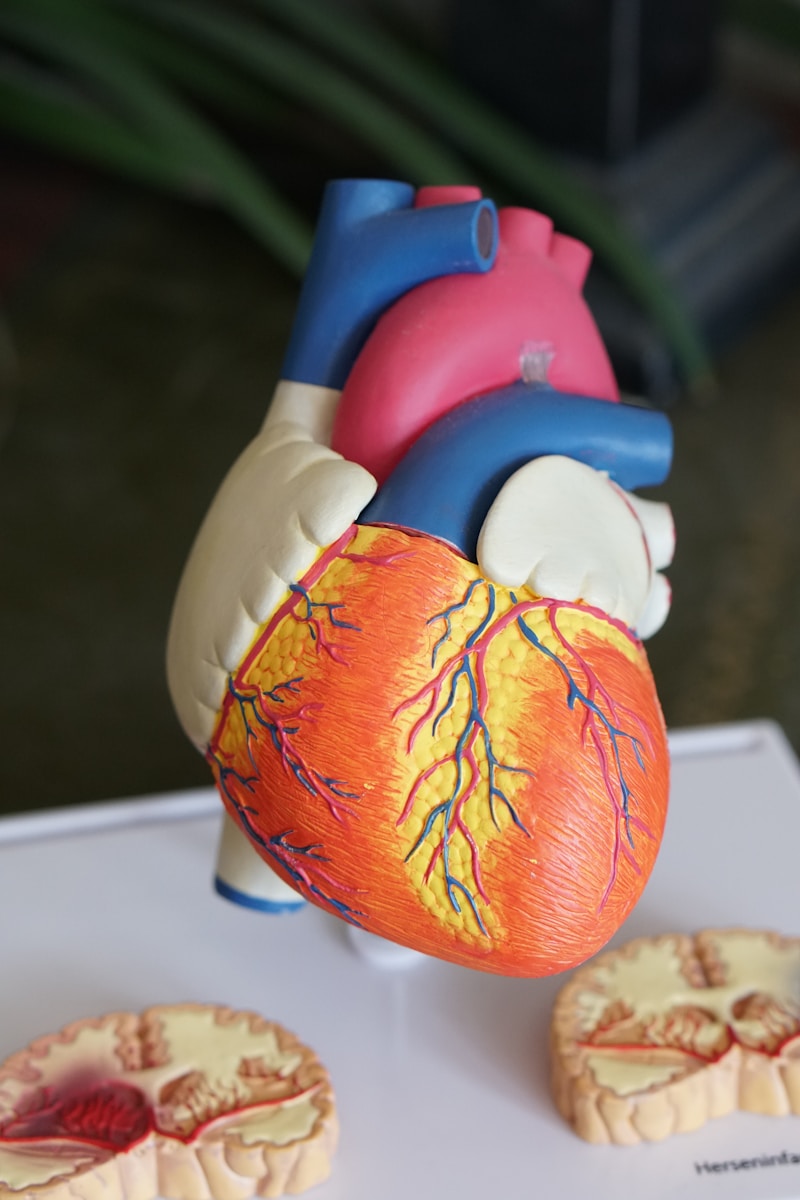
The second most common form of dementia is vascular dementia, and it’s caused by something completely different from Alzheimer’s: damaged blood vessels in the brain. Your brain consumes about 20% of your body’s total blood supply despite being only 2% of your body weight. It is incredibly dependent on a constant, steady flow of oxygen-rich blood.
Vascular dementia occurs when blood vessels in the brain become narrowed, blocked, or damaged. This can happen through small strokes (lacunar infarcts) that may be so tiny you don’t even notice them, chronic high blood pressure that damages small vessel walls, or atherosclerosis (cholesterol plaque buildup) in brain arteries. Each time blood flow is disrupted, the brain cells in that area are starved of oxygen and nutrients — and they die.
What makes vascular dementia particularly insidious is that the damage is often cumulative and silent. Someone might experience dozens of tiny “silent strokes” over years, each one killing a small cluster of brain cells, before cognitive symptoms become noticeable. The person might feel fine while their brain is quietly accumulating irreversible damage. This is why managing cardiovascular risk factors — high blood pressure, diabetes, high cholesterol, smoking — is one of the most powerful things you can do to prevent dementia.
3. The Inflammation Connection: Your Immune System Attacking Your Brain
One of the most exciting areas of dementia research involves neuroinflammation — chronic inflammation inside the brain. For decades, scientists assumed the brain was largely immune-privileged, meaning the immune system left it alone. We now know that’s not true at all.
Your brain has its own immune cells called microglia. In a healthy brain, microglia patrol for threats, clean up debris, and help maintain neural connections. But in dementia, microglia become chronically activated — they switch from protective mode to attack mode. Instead of cleaning up amyloid plaques, overactivated microglia release inflammatory chemicals that damage healthy neurons, accelerate tau tangling, and create a toxic environment that speeds up brain cell death.
What triggers this inflammatory cascade? Chronic systemic inflammation from conditions like obesity, diabetes, gum disease (periodontitis), and chronic infections may all contribute. A groundbreaking 2019 study even found that the bacterium responsible for gum disease was present in the brains of Alzheimer’s patients, suggesting that chronic infections elsewhere in the body can directly contribute to brain inflammation and neurodegeneration. Your brain health is deeply connected to your whole-body health.
4. Genetics vs. Lifestyle: The 60/40 Split That Changes Everything
One of the biggest questions people ask is: “Is dementia genetic?” The answer is both yes and no. Genetics play a significant role, but they’re far from the whole story. The most well-known genetic risk factor for Alzheimer’s is the APOE-e4 gene variant. Carrying one copy increases your risk by 2-3 times. Carrying two copies increases it by 8-12 times. But here’s the crucial point: having the gene doesn’t mean you’ll definitely get Alzheimer’s, and not having it doesn’t mean you’re safe.
Research now suggests that approximately 40% of dementia cases are linked to modifiable risk factors — things you can actually change. The Lancet Commission on Dementia Prevention identified 12 key modifiable risk factors: less education (early life), hearing loss, traumatic brain injury, high blood pressure, excessive alcohol, obesity (midlife), smoking, depression, social isolation, physical inactivity, air pollution, and diabetes (later life).
This is genuinely revolutionary. It means that even if you carry genetic risk factors, your lifestyle choices can significantly alter your trajectory. Studies of identical twins — who share 100% of their DNA — show that one twin can develop dementia while the other doesn’t, proving that genes are not destiny. The choices you make every day about exercise, diet, sleep, social connection, and mental stimulation are constantly either building or eroding your brain’s resilience against dementia.
5. The Brain’s Secret Weapon: Cognitive Reserve
Here’s perhaps the most hopeful concept in all of dementia science: cognitive reserve. Cognitive reserve is your brain’s ability to improvise, find alternative routes, and keep functioning even when damage is occurring. Think of it as the brain’s backup system — the more robust your reserve, the more damage your brain can absorb before symptoms appear.
What builds cognitive reserve? Education, lifelong learning, bilingualism, complex occupations, social engagement, physical exercise, and mentally stimulating activities all contribute. Studies show that people with higher cognitive reserve can have significant Alzheimer’s pathology in their brains (plaques and tangles) yet show no symptoms of dementia. Their brains have built enough alternative neural pathways to compensate for the damage.
This means that prevention isn’t just about stopping the disease process — it’s also about building a brain that can withstand it. Every new language you learn, every book you read, every social connection you maintain, every workout you complete is adding to your cognitive reserve. You’re essentially building an insurance policy for your brain. It’s never too early to start, and it’s never too late to benefit.
Bonus Facts About Dementia
- Sleep is a critical dementia prevention tool. During deep sleep, your brain’s glymphatic system clears beta-amyloid at dramatically higher rates. Chronic sleep deprivation literally allows the toxic proteins that cause Alzheimer’s to accumulate faster.
- Hearing loss is the single largest modifiable risk factor for dementia, accounting for up to 8% of cases. Using hearing aids when needed can significantly reduce dementia risk by keeping the brain’s auditory processing centers active and engaged.
Final Thoughts
Dementia isn’t simply “what happens when you get old.” It’s a complex interplay of toxic proteins, damaged blood vessels, chronic inflammation, genetic susceptibility, and lifestyle factors that interact over decades. The brain damage that leads to dementia often begins 15-20 years before any symptoms appear — which means the choices you make in your 30s, 40s, and 50s are literally shaping your brain’s future.
But here’s the empowering takeaway: up to 40% of dementia cases may be preventable. Regular exercise, quality sleep, healthy diet, social connection, mental stimulation, hearing protection, and managing cardiovascular health aren’t just good advice — they’re your most powerful weapons against one of humanity’s most devastating conditions. Your brain has been protecting you your entire life. Now it’s your turn to protect it.
Sources
- Alzheimer’s Association — 2024 Alzheimer’s Disease Facts and Figures
- The Lancet Commission on Dementia Prevention, Intervention, and Care (2020)
- Nature Reviews Neuroscience — Neuroinflammation in Alzheimer’s Disease
- National Institute on Aging — What Causes Alzheimer’s Disease?
- World Health Organization — Global Status Report on Dementia (2021)